Mapping the unborn
Dr David Lloyd is trying to find his hearts. It's Friday morning in a remote wing of St Thomas' Hospital on London's South Bank, and he's digging around in a box for two plum-sized model hearts, made on a 3D printer the week before.
One, he explains, is the normal heart of a foetus at 39 weeks; but the other, at 35 weeks, has grown abnormally, with the blood vessel wrapped tight around the baby's pencil-thin windpipe. The phenomenon, known as a 'vascular ring', is a congenital condition, present from birth.
When clinicians detect an abnormality like this one at the mother's 20-week ultrasound scan, they might decide to book the birth in at a specialist hospital like St Thomas' so that the baby can get potentially lifesaving emergency care. But the heart is so small at this stage – less than the size of a penny – that about half of congenital heart conditions like this aren't detected. As a result, mothers often don't give birth in hospitals with the right doctors and equipment available, which can dramatically affect the child's chance of survival.
Most read this month
Fiction: Divided we stand, by Tim Maughan How Scotland is tackling the democratic deficit The Long + Short has ceased publishingIn severe cases, a family is rushed to a specialist centre in an ambulance, to await a diagnosis that could change the course of their life. "The advantage of being able to know before that baby is born is huge," says Dr Lloyd, grasping the tiny model heart. "It's so important. And I think this project, not just for the heart but for all the other organs, shows so much promise for how we deal with that."
He's talking about the Intelligent Foetal Imaging and Diagnosis project, or iFind, which started life in 2014. With £10m in grant funding from the Wellcome Trust and the Engineering and Physical Sciences Research Council, iFind appointed paediatricians, software engineers, robotics specialists, and experts in imaging from London hospitals (including King's College London and the Evelina children's hospital at St Thomas') in a massive, seven-year effort to improve 20-week scans for mothers in the UK. The team believe that theirs is the only project of its kind in the world.
If this is successful, it could lift detection rates for abnormalities far beyond what is possible today. "Our goal," says Dr Lloyd, "is to produce a robotic arm that has the dexterity and sensitivity of a human being, knows how to perform a foetal ultrasound, and doesn't look scary."
There are around 700,000 pregnancies every year in the UK. Across the country, an army of sonographers scans every pregnant woman at 12 and 20 weeks to check for abnormalities. They have to be skilled at detecting flaws in tiny unborn babies the size of a small banana, often while the baby wiggles around, using technology first applied in the 1950s.
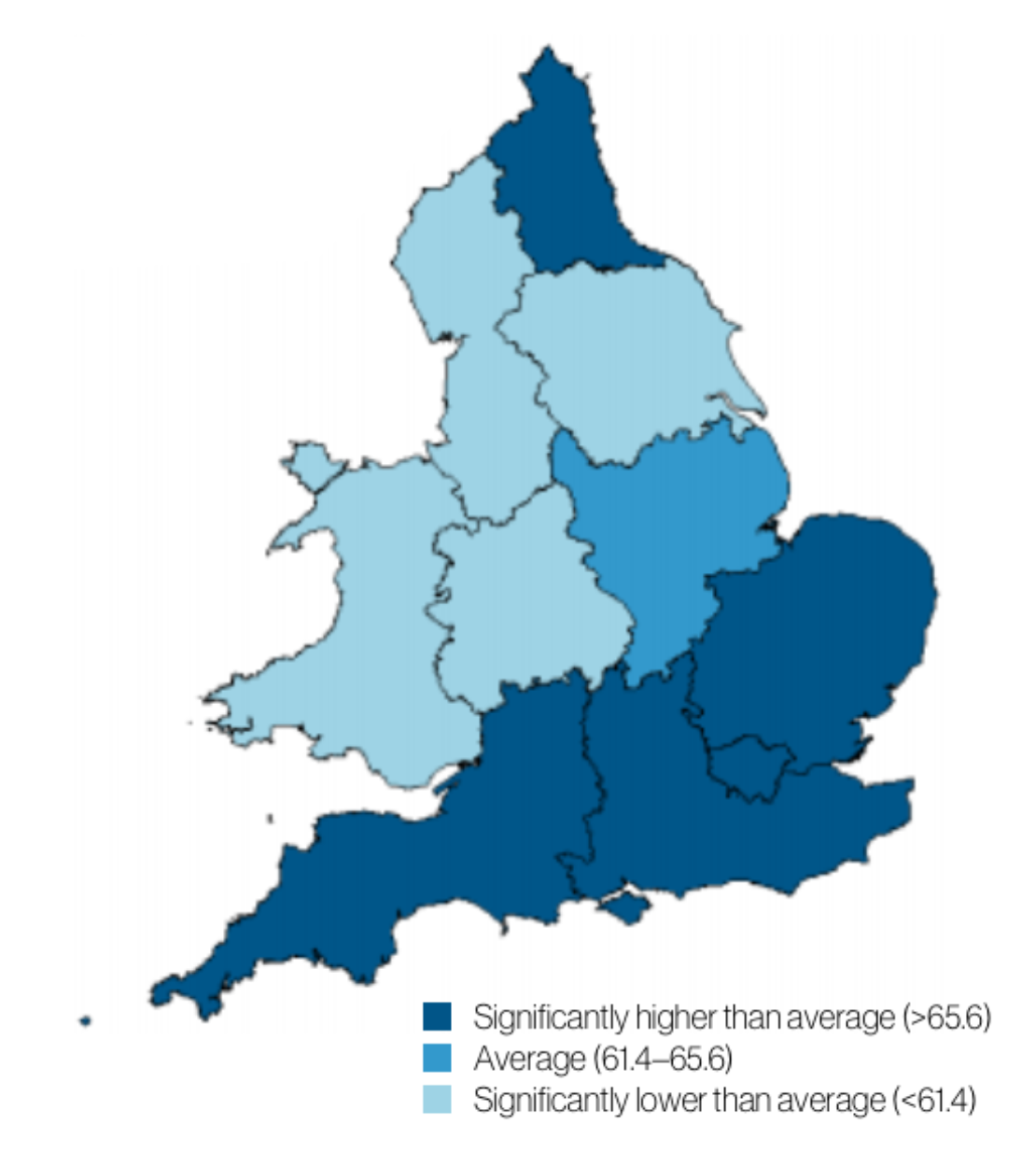
Even experts miss things under these conditions. Target rates for detecting abnormalities range from 98 per cent for something like anencephaly, which can be caused by the Zika virus, to 50 per cent for complex issues like those related to the heart. In national referral centres like St Thomas', such problems are often picked up by teams of expert sonographers and doctors who have probably dealt with them before.
Sonographers have to be skilled at detecting flaws in tiny unborn babies the size of a small banana, often while the baby wiggles around, using technology first applied in the 1950s
But in some less specialist hospitals, more than half of these problems are missed. "Fifty per cent means you've got only one chance in two that your baby is detected," says Professor Joseph Hajnal, an expert in foetal Magnetic Resonance Imaging (MRI) from King's College London who is also co-leader of iFind at St Thomas' Hospital. "In some places, detection rates might drop to 10 per cent," he adds. "If you think about [there being] a 90 per cent chance that we're not going to see something essential to the development of your baby, that's a pretty upsetting thing. It's not the way people [like to] think about modern healthcare."
iFind aims to raise detection rates in those hospitals which most need it. Part of the project involves creating an 'atlas' of a healthy foetus. The team started by collecting anonymised ultrasound data from 10,000 patients. In the second part of the data collection process, 500 volunteers are being signed up to visit the clinic at St Thomas' on Fridays for an additional ultrasound and an MRI scan. "You'll see what they go through today," Dr Lloyd says. "500 [volunteers] is quite a lot."
We leave the office and head to the examination room, where Dr James Housden, a robotics researcher, and Jackie Matthew, a sonographer, both from King's College London, are readying the equipment for the day ahead, watched by a student and a project administrator. More equipment and people are already in the room than you'd get at a normal ultrasound scan. A state-of-the-art ultrasound machine is connected to two bulky probes, each fitted with 3D ultrasound technology and motion sensors so that they can track the clinicians' movements.
Dr Housden boots up a separate computer, further from the bed, to collect data about how the probes are moving. He tells the team how the previous week, engineers had trialled robotic arms fixed to the side of the bed to scan a dummy belly, with some success. Machines can offer much more precision than humans, but it's not as simple as that. The robot has to be able to twist and flex, to apply the right pressure and to tell which parts of the belly and the baby to scan, all without hurting the mother. To build a robot that can do that, Dr Housden first has to record data about how humans do it.
Their patient, Rebecca Hooper, arrives, and is introduced to everyone in the room. She had been asked whether she wanted to take part in iFind at her 12-week scan. She had agreed to do it, she says, because she was a science graduate who at one time had considered a career in medicine, and was fascinated by medical research. Rebecca feels strongly that research projects should improve technology for babies in the future, not least because when her mother was pregnant with her, the doctors missed something. "When I was born the doctors told my parents that I had mild spina bifida," she says.
"It doesn't affect me from day to day," Rebecca says. "But I thought it was really interesting that my mother, when I asked her, said they only had one scan in the 1980s. They weren't allowed to look at any pictures. They were just told the baby was there; and that's all they knew until they gave birth." Detection rates for spina bifida are now greater than 95 per cent.
Our goal is to produce a robotic arm that has the dexterity and sensitivity of a human being, knows how to perform a foetal ultrasound, and doesn’t look scary
Rebecca's scan couldn't be more different to her description of her mother's. Jackie squirts jelly on Rebecca's belly and angles the screen towards her so she can see what's going on. Using a single probe, Jackie tracks the parts of the baby: heart, head, spine. Even small details show up on the screen, like the kidneys and eye sockets. Rebecca's surprised how high up the baby is. It looks like there's loads of space for it to move around in.
Dr Housdon records Jackie doing several 'sweeps' of Rebecca's belly. Jackie moves the probe in a straight line so that the ultrasound beams build a complete picture of the baby inside.
"Your baby's being lovely," Jackie reassures her. One of the benefits for the volunteers taking part in the project is that they get to take home a whole set of 2D and 3D images from the ultrasound, as well as some video material of the baby from the MRI scan later in the day. Jackie tries to get some good images of the baby's face for Rebecca.
Dr Lloyd steps in to take some more detailed images of the baby's heart. Then Jackie returns to the seat in front of the screen while Dr Lloyd takes a second probe round the other side of the bed. They squeeze more jelly on Rebecca's belly and practise making images of the heart from two different angles. Dr Housdon records the images on his computer. The whole scan takes about an hour.
"There were lots of people in there," Rebecca says when the scan is over. "Normally when you have a scan it's just you and your partner and it's quiet. But it wasn't as daunting as I thought." She has a few hours to kill now before the MRI scan, and heads off to get lunch.
The images created by ultrasound can prove extraordinarily useful to trained eyes, but the quality can vary enormously. Ultrasound has to be able to 'see' through the body to the parts of the baby the clinicians want to look at, which isn't always easy. Their success depends on the age of the baby, how it is lying in the womb, the size of the mother, and many other factors.


By contrast, MRI, which uses a strong magnetic field and radio waves to produce images, isn't so limited. It can 'see' right through bone, muscle or fat and in some cases provide images far more detailed than ultrasound. But it's expensive. If you've got to do several hundred thousand screenings a year, the cost difference between an ultrasound and an MRI scan is huge. That's why it is only used to diagnose problems if clinicians think something might be wrong. In iFind, it's being used to build the foetal atlas that the robotic arms will eventually use to compare with live images from their scans.
After lunch, Rebecca changes into a gown and an MRI specialist takes her through the preliminaries. They double-check her body for metal and jewellery. She's given headphones playing commercial radio to block out noise and to keep her entertained. For an hour she'll be kept immobile under heavy pads containing the coils that receive MRI signals from the giant magnet in the middle of the machine.
Unborn babies can't wear headphones, of course. But research has shown that the sound doesn't pass through the womb. The heart rate of babies undergoing MRI scans doesn't change, which has reassured researchers that they're not too bothered by the process.
While Rebecca is having her scan, another team of researchers gathers moving images of her baby from a little lab looking into the MRI room through a window. It doesn't look like there's much to see from the window; but on the researchers' screens, Rebecca's body appears in slices. Her digestive organs are squashed around her womb, allowing access to a perfect image of her growing baby.
Have you subscribed to our weekly updates?
NewsletterDr Lloyd homes in on Rebecca's stomach, then the baby's miniature version, then mother and child's kidneys and bladders. His trained eye can see the atriums and vessels of the baby's heart. If he can get the right image 'slice', he can spot an abnormality like a vascular ring straight away. The problem with MRI is that when the baby is moving, the image slices don't merge to give a good enough 3D image from which the doctor can diagnose problems.
The team takes multiple images of Rebecca's baby over the course of an hour, making sure to save some video footage to a disc for Rebecca to take home.
We head back up to Dr Lloyd's office. One of the early successes of the iFind project has been applying algorithms to MRI images that can account for a baby's movements. "That's how we managed to make this heart," says Dr Lloyd. "From an MRI scan that we were able to 'correct' to make a 3D model."
The team is looking at ways to apply this algorithm more widely, to give doctors much clearer MRI images of babies' organs to work from. Professor Hajnal says these kinds of achievements are just as important as creating a foetal atlas, or robots to assist with ultrasound scans. "In the end, although we might come up with something that we think is utterly brilliant and will have a huge impact on improving detection rates, it might be too expensive. But something quite simple that we figure out might allow something quite close to current technology to be incrementally better in a way that is worthwhile to do," he says.
Ten years ago, researchers wouldn't have been able to work on this project, and in 10 more years it will be different again. While the team might develop ideas that cannot currently be deployed, these may become possible with the march of time. In the meantime, developments like the movement algorithm are already informing the work of scientists like Dr Lloyd, helping to raise those 50 per cent detection rates to give new babies and their parents a better chance at a normal life.
"This project will make a really positive difference not just for pregnant mothers, or for their babies just after they are born," says Dr Lloyd, "but for the lifetime of those babies, and [in turn] their families too." With that, he packs the two tiny hearts away in their box.