Obstetrics for beginners
It's my first go at delivering a baby by caesarean section – and the foetal head is impacted, jammed in its mother's pelvis. To be honest I'm struggling.
Incisions have been made in the lower part of the mother's abdomen and womb. I've pushed my gloved hand inside and managed to slide my fingers between the baby's head and the surrounding uterine tissue. But it's difficult. The baby is tightly wedged in. I've had to push hard to get my hand to the far side of its head, and even though I'm now cupping and grasping it in the approved manner, I can't seem to pull it out. Dare I grip its head more firmly? Dare I pull harder?
The baby's mother – she's called Debra – remains impassive throughout these agonised fumblings. Her face reveals nothing of what she may be feeling. But then Debra has no feelings. Indeed she has no face…
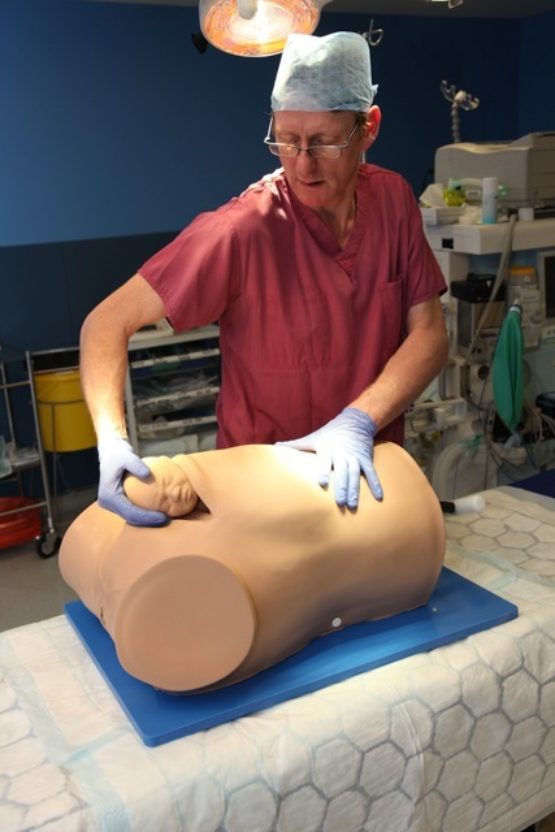
So you can stop worrying. Debra – Desperate Debra to use her full trade name – is a simulator designed to help doctors practise their skill at dealing with impacted foetuses: babies that get stuck trying to exit the womb by the normal route. She comprises the lower two thirds (ie from the mid-chest region downwards) of a life-sized but limbless female torso made of flesh-coloured silicone rubber. She comes with a vulva, a pre-cut incision in her abdomen and, most importantly, a uterus containing a foetal head that should, in the normal way of things, be free to emerge between her legs. But this fetus is going nowhere until an obstetrician – or in this case me – can successfully grasp and pull it out.
The clever and sophisticated simulator I'm playing with started life as a lash-up in an obstetrician's home workshop: a Heath Robinson-style contraption barely recognisable as a model of the human body. But it wasn't at that stage intended as a simulator for training medical staff. Its sole purpose was to test the effectiveness of a novel device called a Tydeman tube. Paradoxically, although the testing equipment, Debra, is now commercially available, the device it was intended to test has yet to reach the market.
The inventor of the tube and of Desperate Debra is Dr Graham Tydeman, a consultant in obstetrics and gynaecology at Victoria Hospital in Kirkcaldy, Fife. Only after he'd built Debra did he realise that she might serve a purpose beyond his original intention. His is a decade-long tale of inspired insights, thwarted aims and shifting purposes; but with a good outcome. Although the Tydeman tube is still in gestation, Desperate Debra herself is now thriving.
To understand the desperation of Debra and how the Tydeman tube might help to relieve it requires a brief foray into basic obstetric knowhow. Evolution has endowed us with heads proportionally so large that even when labour runs according to plan, the delivery process involves a bit of a squeeze. For the baby's head to get stuck on the way out may not be usual, but it's by no means a rarity.
The standard response is to perform a caesarean section. Every year some 160,000 babies are born in the UK this way, with almost two thirds of them classified as emergencies. One audit has suggested that roughly 8,000 babies get stuck and have to be delivered by caesarean at a stage when their mothers are fully dilated. "Some of the babies will be so close to coming out by the normal route," says Tydeman, "that it's then difficult to get them back up and remove them through the hole in the woman's tummy." Which women are most at risk of this setback seems to be largely unpredictable. "We just observe that it happens… It's been discussed in the medical literature since the 1940s, but until 10 years ago, and throughout my training and most of my life as a consultant, it wasn't really talked about."
The skin was made out of a neoprene wetsuit fixed to plastic tubing; the head was cast in silicone; the rest comprised old springs and other bits of stuff lying around his workshop
Considering the universality of childbirth, impaction and the best way of dealing with it are topics that seem to have gone remarkably unstudied. "There are strong opinions about why it happens and what to do, but very little research evidence," says Tydeman, adding that many of these opinions are contradictory.
In a protracted birth that's destined to end with a caesarean, the longer the labour is allowed to go on before the obstetrician decides to intervene, the greater the likelihood that the baby's head will become impacted. However, concern over the rising number of babies born by caesarean has made doctors more wary of doing them – one consequence of which is that medical staff may allow a difficult birth to continue for longer before they resort to surgery. This could be boosting the frequency of impaction. But, again, no one is certain.
When obstetricians doing planned caesareans slice open a mother's womb, what they usually see is the baby's head. By slipping a hand round and below it they can easily guide the baby out. "When you do a caesarean for an impacted baby," says Tydeman, "you make the incision in the same place, but what you might come across is a shoulder because the baby's so much further down [the birth canal]." As I'd discovered for myself, sliding a hand around the baby's head is then far more difficult. "It makes your fingers hurt," says Tydeman. "It makes your pulse rate go up to about 200, and you break out in a sweat because know you've only got about five or 10 minutes before there are serious consequences. The clock is ticking."
If a baby's head is jammed down in the mother's pelvic region, common sense suggests that it might help if a second person gives a gentle backward push on the area of its head visible through the mother's dilated cervix. "In our unit," says Tydeman, "when the woman is fully dilated and you'd expect the baby to come out normally [but it doesn't]… a registrar will be asking for a push-up about one in five times." Although registrars are doctors still in training, they're nonetheless experienced; which suggests requests for push-ups during unplanned caesareans are far from uncommon. The Tydeman tube is a gadget intended to make this manoeuvre safer and more effective.
Creativity and innovation have many unlikely sources. What seems to have inspired Tydeman to develop his device was the characteristic sound of a Wellington boot being pulled free of wet, muddy ground: a slurpy, sucking, gurgling noise. When an impacted foetal head is pulled free of the uterus it's often accompanied by a similar sucking noise, the result of air rushing in between the obstetrician's fingers to fill the space vacated. "What occurred to me years ago was that if the air can't get in, why not put a tube up into the vagina so that it can get in from below the baby's head." From time to time, if he felt he felt the baby might stick, Tydeman would slip a length of sterile silicone tubing through the woman's vagina and up into the womb next to the baby's head. Allowing air in by this route would release any suction forces tending to hold it where it was.
Tydeman didn't do much with the idea until 10 years ago when one trainee, who was experiencing real difficulty getting heads out, prompted him to think again about the problem. Around the same time, he met professor of obstetrics Andrew Shennan and consultant midwife Annette Briley, both of the Women's Health Academic Centre at St Thomas's hospital. Between them they came up with a device – the Tydeman tube – to make pushing on the foetus more controlled while simultaneously releasing any vacuum that might be holding it in place.
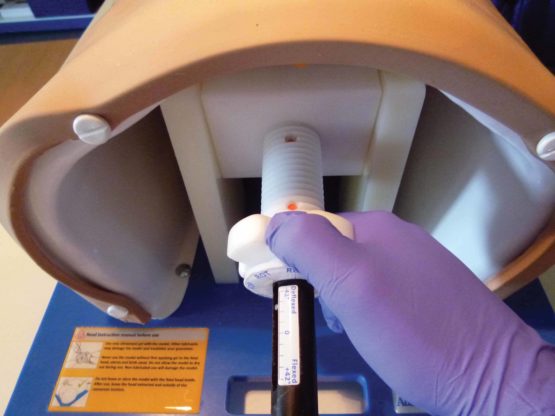
The instrument is made up of a rigid plastic tube opening into a softer silicone cup. Pressure to the foetal head is applied using four pads projecting forward from the cup's interior. Holding the device by the tube, the user places the cup against the part of the head exposed through the dilated cervix, and presses. This pushes the baby back up into the uterus while releasing any suction pressure that may have been holding it, so allowing the obstetrician to extract it more easily. Because pressure is distributed equally between the four pads with a greater combined surface area than that of a user's fingertips, the risk of inadvertent damage is minimised.
The team found some money to employ a product designer who used computer-aided design technology and 3D printing to make a prototype. "We were at the point of getting one made in silicone," says Tydeman, "when we realised that before we started experimenting on women we really ought to test it on a simulator." No such simulator existed – so he decided to make one himself.
That Tydeman was able to do this comes as no great surprise once you've glanced at his website. His career may be rooted in medicine but his interests encompass sculpture, furniture making and much else. He works in wood, glass, metals and plastic. "I've got a big workshop with a lathe and a forge," he says. "I make stuff. I always have, ever since I was a child. My dad was a woodwork teacher, my mum was very creative with fabric."


Although tests carried out with the Debra prototype showed that the tube would work as intended, Tydeman and his colleagues then faced what he calls a kind of medical catch-22. "We had the tube finished about three years ago… but we were more interested in trying to save lives than selling a product. We thought that the right thing to do before commercialising it was to be sure we'd got the best design." They tried it on a dozen or so women in labour, and concluded that it did what it supposed to. But they held off trying to market it because they wanted to do more extensive, more rigorous clinical studies.
This presented a problem. "If you've applied for research money," says Tydeman, "but you've already got what seems to be a commercially viable design, potential funders are going to say that the company aiming to sell it should pay for the work." On the other hand, commercial interest is easier to drum up if you've already got evidence that a device is safe and effective.
That said, the team didn't want to leave the tube sitting on the shelf. So they eventually decided to go ahead and find a commercial partner willing to manufacture and market it. They have now identified one, and are fairly confident it will soon be in production. With sufficient users it should then be possible to compile factual – as opposed to anecdotal – evidence of benefit. Not ideal, Tydeman concedes, but the best they can do at present.
In the meantime, back to Desperate Debra: so named, Tydeman says, not after any particular person but because the appellation is memorably alliterative. He put together the original Debra in a weekend. The skin was made out of a neoprene wetsuit fixed to a scaffolding formed from plastic tubing he'd found 20 years ago in skip outside a Glasgow pub; the head was cast in silicone from a model he'd made in plasticine, and the rest comprised old springs and other bits of stuff lying around his workshop. "It wasn't actually that difficult," Tydeman says.
When originally conceived, remember, Debra was simply a means of testing the effectiveness of the tube. What she looked like was neither here nor there. It was only once Debra was reborn as a teaching aid that she needed sprucing up.
Tydeman can remember the exact moment when the idea of her having a greater role dawned on him. "I was on the sleeper train down from Scotland to London," he says. "Debra was with me because the first Tydeman tube had become available at St Thomas's… It was about midnight, I'd had my free whisky and I suddenly thought, 'Blow me! Even if the tube doesn't work, Debra could be useful as a teaching aid'."
Sign up to our newsletter
The following morning, at St Thomas's, Tydeman asked a visiting professor of obstetrics to have a look at Debra and tell him what she thought. She put her hand into Debra's womb, grasped the foetal head and said it felt just like the real thing. "Terribly flattering," Tydeman laughs.
With a grant from the Guy's and St Thomas's Charity fund they made Debra more presentable. Tydeman showed the prototype to Adam Rouilly, an established company specialising in medical models and simulators. They were impressed. A year later, the first of Debra's smartened-up sisters was on the market.
In Debra as she is now, the precise extent and nature of her desperation can be fine-tuned according to need. The foetal head inside her uterus can be moved to mimic the various positions that an unborn baby may adopt. By tightening a spring inside Debra's body, it's also possible vary the degree of impaction from mild to so severe that the head is virtually impossible to extract. In this way she simulates the full range of difficulty that obstetricians are likely to encounter.
So how valuable in training medical staff is a simulator like this? Very, according to Annette Briley. Imagine it's the middle of the night and an unplanned emergency caesarean is required: "Some poor junior doctor might find himself trying to manage it on his own." To have practised the knack of extracting a firmly impacted baby from a simulator is lot better than first honing your skill on a real woman.
At St Thomas's, midwives in training also get an opportunity to practise on Debra. The chances that midwives will find themselves having to do the actual extraction of an infant are slim; but they're quite likely to be asked to help the obstetrician by pushing a stuck baby from below. Debra's anatomy allows them to practise this skill; and to learn where and how hard to push on the infant skull. "Any practice you've done in the cold light of day will help you stay calm and composed in an emergency, and that's what we're aiming for," says Briley.
Medicine as a whole has an oddly ambivalent relationship to innovation
It's still too soon to make a final judgement about Debra’s impact. "When we first brought Debra out," Briley recalls, "some of the really experienced professors said things like, 'We always managed without one. Why would you need this?' But ask them to have a go at using it and then they admit it's really good." Medicine as a whole has an oddly ambivalent relationship to innovation. Some new findings, techniques or equipment take years to penetrate the profession; others are seized upon immediately.
A proper study of the clinical effectiveness of the Tydeman tube will necessarily involve women giving birth. Assessing the value of Debra as a simulator didn't require human subjects; and the team has already conducted such a study. Thirty obstetricians, from three NHS maternity units and with varying levels of experience, took part. They all received a brief explanation of how Debra works, and were then asked to try a timed removal of the foetal head at three different levels of difficulty. Overall, 87 per cent reported that the simulator offered a realistic experience of dealing with an impacted head, and 93 per cent thought it would be valuable as a training device.
The use of simulators to teach technical skills is now common in medical schools. You can learn to sew up a knife wound, catheterise a bladder or intubate an airway. You can practise cardiopulmonary resuscitation or ear syringing or even go through the motions of a keyhole surgical procedure. The technology required to do these things may cost a few pounds, or tens of thousands. Either way, given that most of these devices were invented during the past three or four decades, it comes as something of a surprise to learn that simulation for medical purposes can be traced back as far as the Chinese Song dynasty of 960-1279 AD.
Explore
Mapping the unborn: the future of ultrasound scans Home Depot heart surgery How the Beatles gave us the CT scanOne of the treatments of choice in that era was, naturally, acupuncture. But how to teach tyro-acupuncturists where to place the needles? Simple. A life-size bronze statue dotted with small holes indicated the points of insertion. And how then to test the students' grasp of their subject? If the statute was hollow, filled with liquid and given an outer coating of wax to mask the holes, a correct needle insertion would be followed by a leak.
Given the universality of childbirth it's no surprise that, then as now, the womb turns out to be the most simulated of our organs. For the benefit of 18th-century midwives and doctors-in-training, the Bologna surgeon Giovanni Antonio Galli devised a birthing simulator comprising a glass uterus supported by an artificial pelvis and containing a flexible foetus. Trainees had to deliver the baby while wearing a blindfold. Only the tutor could witness the fumbling of their hands.
As the material for a convincing simulation, glass clearly has its drawbacks. But another 18th-century contraption used a pink cloth-covered mannequin comprising a female torso complete with genitalia, a set of implantable foetuses of various ages, and even – a real coup de théâtre, this – a facility for exuding suitably coloured liquids at the appropriate moment.
Oddly, as medicine became more scientific, most of these devices fell by the wayside. As an academic review of these and other devices has pointed out, much of the 20th century was something of Dark Ages for simulation. Its value in professional training has had to be rediscovered: an endeavour in which inventive people like Graham Tydeman, sometimes with workshops rich in discarded junk, are still fruitfully engaged.